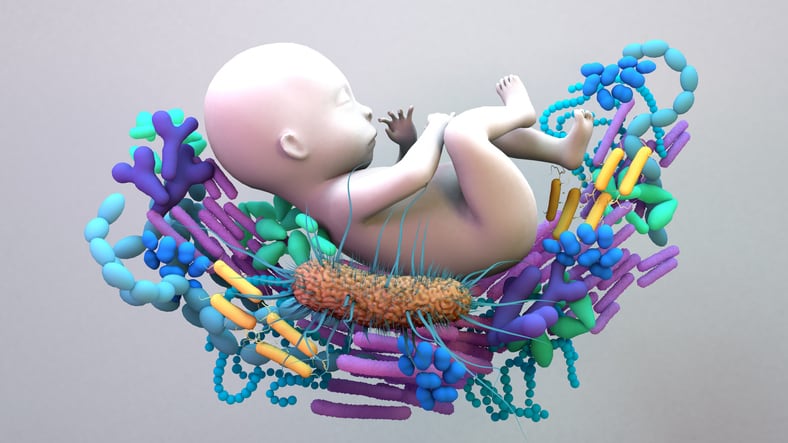
A recent publication in the Journal of the American Heart Association (JAHA) reports an association between the composition of the infant gut microbiome, especially the presence of Bifidobacterium species, and blood pressure measured in early childhood.
The researchers’ conclusions suggest these findings offer strategic direction for the development of next-generation probiotics, prebiotics and synbiotics aimed at early-life health.
Study overview
The study, “Infant Gut Microbiota and Childhood Blood Pressure: Prospective Associations and the Modifying Role of Breastfeeding,” examined a Danish birth cohort of 736 mothers, followed by 700 of their children, and found that “infant gut microbiome diversity and composition are prospectively associated with child blood pressure at three and six years of age.”
Notably, the presence of specific Bifidobacterium species within the first month of life was shown to play a key role, particularly when coupled with breastfeeding for at least the first six months of life.
According to the authors, “alpha diversity and specific Bifidobacterium microbes showed protective associations with blood pressure, especially when infants are breastfed for at least six months.” The study further found that “breastfeeding and the presence and abundance of Bifidobacterium within the first month of age showed interactive associations on BP at three years.”
The findings support a broader understanding of the gut–cardiovascular axis and suggest that early microbial colonization may influence metabolic and cardiovascular trajectories.
The authors concluded: “Our study provides pioneering evidence linking infant gut microbiota with BP at three and six years of age, highlighting early life as a critical period for microbiota‐focused interventions aimed at preventing hypertension.”
Industry expert weighs in: supplements that do not contain Bifidobacterium ‘are missing an opportunity’
NutraIngredients spoke with Stephanie Culler, PhD, co-founder and CEO of Persephone Biosciences, Inc. Commenting independently, she stated that the findings “strengthen that [infant gut–cardiovascular] link by demonstrating an association in humans.”
While experimental models have suggested that microbiota may affect blood pressure via immune modulation, this study represents one of the first to confirm such a relationship in a pediatric human cohort, according to its authors.
“It is not surprising that this is associated with Bifidobacterium in infants, as they play an outsized role in infant immune development,” said Dr. Culler. “The reliance of the association on breast milk hints at a potential role for human milk oligosaccharides (HMOs), although additional studies would be needed to understand that relationship.”
Dr. Culler emphasized that these results underscore a critical direction for innovation in the supplement space. “This data further suggests that the dietary supplement industry should be focusing on infant-associated Bifidobacterium and the prebiotics that support them: HMOs,” she said.
Further, she continued, “a growing body of evidence—this paper included—suggests that the long-lasting impacts of the microbiome are driven by specific Bifidobacterium, and supplements that do not contain them are missing an opportunity to positively affect long-term health.”
Scientific innovation and product development
In their conclusion, the authors acknowledged a growing need for advanced tools to refine microbiome-targeted interventions. In particular, they wrote, “future research should focus on shotgun metagenomic and metabolomic analysis to identify specific infant gut microbes, particularly Bifidobacterium species, and microbial metabolites associated with cardiovascular health in childhood.”
Dr. Culler echoed this direction and described how companies are responding. “Most probiotics have been around for decades, since before accessible sequencing existed,” she explained. “Today, small companies like ourselves are attempting to redefine the probiotic space by using cutting-edge techniques to truly understand what is missing in modern microbiomes.”
She added that Persephone Biosciences leverages deep sequencing to differentiate between Bifidobacterium strains: “We push sequencing as far as it can go to understand the subtle differences between Bifidobacterium.”
While acknowledging innovation from larger firms, Dr. Culler noted that smaller players often bring speed to market. “Larger companies also appreciate the importance of innovation in the space and are doing great work to support the next generation of probiotic supplements, but the speed with which small companies like ourselves move means we can get innovation to the consumer sooner.”
Navigating regulatory complexity
As researchers continue to expand the body of research supporting the link between gut microbiota and cardiovascular health, regulatory guidance and clarity are becoming increasingly necessary for manufacturers of pediatric-focused supplements.
Dr. Culler advised that “the best way to ensure that consumers are receiving a high-quality product that does not overreach in terms of claims is to consistently perform exceptional clinical research and also be in contact with the FDA so that they can provide the proper guidance.”
She concluded, “The role of the microbiome in health is huge and undeniable, and consequently a complex legal space to navigate for a supplement company.”
Source: Journal of the American Heart Association doi.org/10.1161/JAHA.124.037447 “Infant Gut Microbiota and Childhood Blood Pressure: Prospective Associations and the Modifying Role of Breastfeeding.” Authors: Tiange Liu, PhD, MBBS et al.