Non-alcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease with an estimated global prevalence of 25%. Treatment options for the NAFLD are limited and mainly revolve around lifestyle interventions but it has to be treated early owing to its tendency to progress to further complications.
It has been suggested that disturbances in the gut microbiota composition lead to gut dysbiosis, causing a disruption to the arrangement of the adjacent intestinal epithelial cells by loosening tight junctions, which subsequently triggers the response of adaptive immunity. Tight junction proteins, such as zona occludens-1 (ZO-1), play a significant role in maintaining the monolayer integrity of epithelial cells.
The translocation of microbial endotoxins, such as lipopolysaccharides, have been shown to induce steatosis, inflammation, and fibrosis, as well as elevated inflammatory cytokines, such as TNF-alpha (TNF-α).
Therefore, probiotics present a possible target of treatment by manipulating the gut microbiota and modulating intestinal permeability and local mucosal inflammation.
The current pilot study was conducted in an aim to assess whether twice daily probiotic supplementation (Hexbio, comprising MCP BCMC strains) over a six month period can improve hepatic steatosis, fibrosis, and other clinical biomarkers in NAFLD patients.
Since the small intestine is responsible for most nutrient absorption and digestion, the researchers also explored the role of the small intestine in the development of NAFLD. Therefore, the team also determined the effect of probiotics on changes in the expression of CD4+ and CD8+ T lymphocytes (mucosal immune function) as well as ZO-1 (small intestinal barrier).
The study
The team conducted a randomised, double-blind, placebo-controlled study involving 32 patients from the Universiti Kebangsaan Malaysia Medical Centre (15 in the probiotics group, 17 in the placebo).
At baseline measurement, patients’ comorbidities (diabetes mellitus, hypertension and dyslipidemia) were recorded and baseline dietary pattern was assessed using a Food Frequency Questionnaire (FFQ).
A set of blood investigations was carried out before and after the intervention to analyse the level of steatosis, fibrosis, and inflammation.
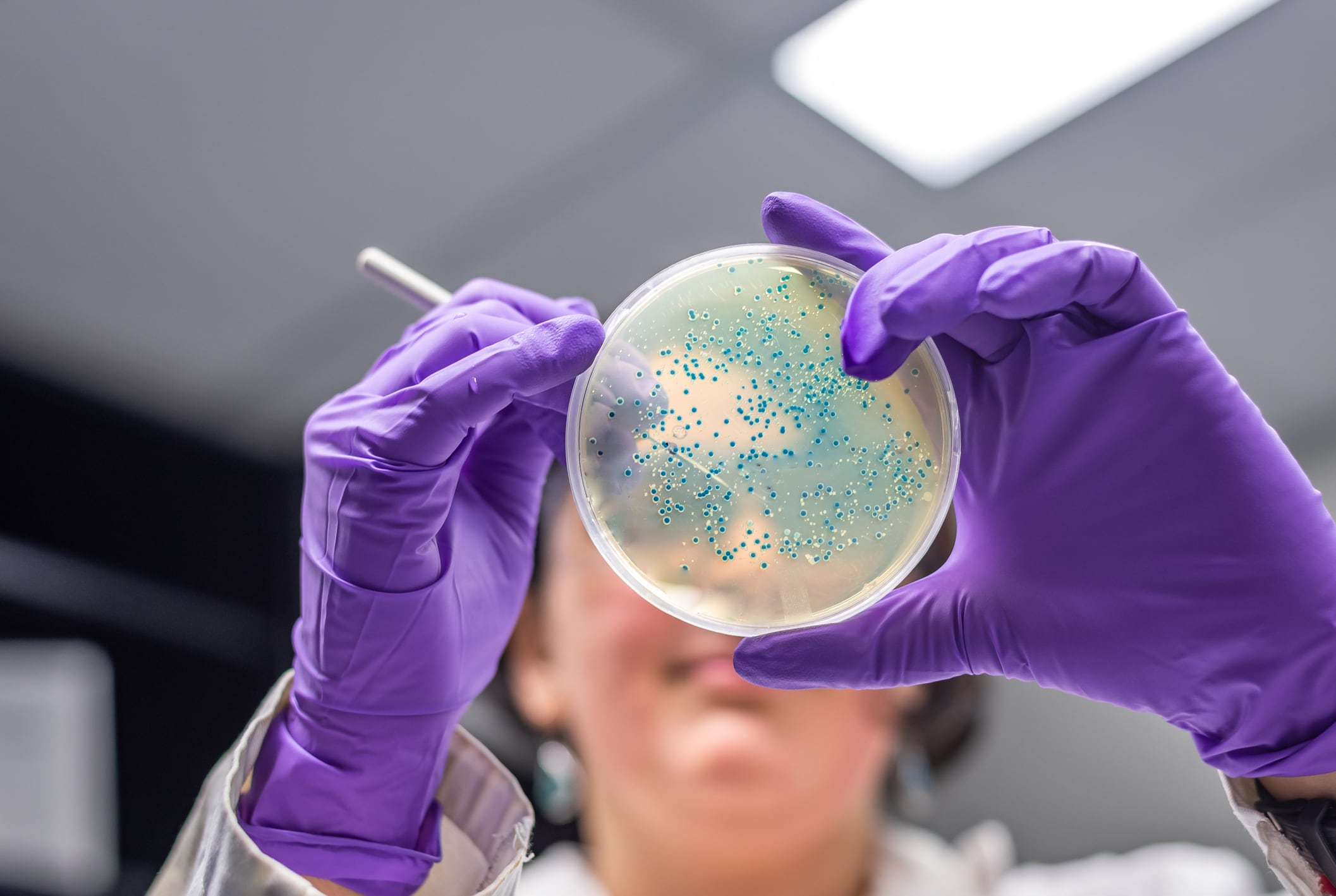
Duodenal samples (the second part of the duodenum) from the NAFLD patients were obtained by performing oesophagogastroduodenoscopy (OGD) before and after the intervention.
A FibroScan 502, manufactured by Echosens (Paris, France) was used in the study to obtain the liver stiffness measurement and the controlled attenuation parameter.
Results
The team found the use of the probiotics for a 6-month duration did not show any significant clinical improvement in NAFLD patients, namely hepatic steatosis, fibrosis, and activity scores, or biochemical blood tests.
However, in the small intestine, probiotics seemed to be able to stabilise the mucosal immune function, as shown by the reduced expression of CD8+ T lymphocytes in the placebo group but not in the test group.
Additionally, probiotics were able to protect NAFLD patients against increased intestinal permeability, unlike in the placebo group. Therefore, the researchers conclude probiotics might play a complementary role in treating NAFLD.
The researchers say further studies with larger sample sizes, a longer duration, and different probiotic strains are needed in order to evaluate the real benefit of probiotics in the management of NAFLD.
Source: Nutrients
Mohamad Nor, M.H., Ayob, N., Mokhtar, N.M., Raja Ali, R.A., Tan, G.C., Wong, Z., Shafiee, N.H., Wong, Y.P., Mustangin, M., and Nawawi, K.N.M.
"The Effect of Probiotics (MCP® BCMC® Strains) on Hepatic Steatosis, Small Intestinal Mucosal Immune Function, and Intestinal Barrier in Patients with Non-Alcoholic Fatty Liver Disease"
https://doi.org/10.3390/nu13093192 (registering DOI)